All About Bedwetting

The medical term for bedwetting is “Enuresis”, it means involuntary urination. It is most common in young, and adolescent children. It’s worth noting that Enuresis can be broken down into 2 types; Primary Enuresis and Secondary Enuresis.
Primary Enuresis is usually used to describe the condition where a child has never stopped wetting the bed or has only stopped for a very short time.
Secondary Enuresis is usually used to describe the condition where a child has stopped wetting the bed for 6 months, but has then relapsed. The causes of Primary Enuresis and Secondary Enuresis can be quite different.
There isn’t usually an obvious cause of either type of Enuresis, but reasons could include:
The child is a very deep sleeper, the signal informing their brain that their bladder is full isn’t strong enough to wake them up to go to the toilet.
An overactive bladder that can only hold a small amount of urine, this results in the child needing to urinate more frequently.
The child produces more urine than their bladder can hold.
Much rarer causes of Enuresis, and in particular Secondary Enuresis can include emotional distress, or an underlying health problem.
Social problems, or upheaval suffered by the child, such as bullying, or a change of environment such as moving school can also be causes.
Health problems such as a urinary tract infection or type 1 diabetes may also be causes.
However, the reality is that for the vast majority of bedwetting cases, the child does not have a physical, or psychological problem. Their Enuretic problem simply stems from the fact they are unusually deep sleepers. They are normal and healthy children, but simply haven’t fully developed the necessary subconscious reflexes they need to wake up from this deep sleep. Basically, pressure builds up in the bladder as it fills with urine, when it’s nearing full a signal is sent to the brain to inform it that the bladder needs to be emptied, in a fully developed person, the subconscious receives and reacts to this signal, waking them up. With Enuresis caused by deep sleep, either the signal sent to the brain is too weak to wake the person, or the subconscious reflex in the brain hasn’t fully developed to register and react to the signal.
The good news for these children, the THERApee bedwetting solution is ideal; it works to train these reflexes through the use of the alarm system, and positive re-enforcement behavioural modification through the interactive online software.
How common is Bedwetting?
It is considered normal for a child to grow out of bedwetting between the ages of two and four. However, about 25% of children still wet the bed at four years of age, by age five the percentage of children still wetting the bed falls to about 20%, by age six it’s 15%, by age ten it’s 8%, and by age fourteen it’s 8%. The percentage of the population aged eighteen and over still wetting the bed is about 2%.
Is Bedwetting more common in Boys or Girls?
Boys are more likely to suffer from Enuresis than girls. About two-thirds of Enuresis cases are reported for boys, and only one-third for girls. However, by the age of seventeen, the proportion of boys with the condition drops to one-third, and rises to two-thirds for girls. There is no clear reason why the proportions change as children get older, but some reasons suggested for this include the fact that girls mature more quickly than boys in their early years. During adolescent years, it is generally accepted that girls have more emotional factors which may play a part when compared with boys.
Is Bedwetting Inherited?
According to Howard Bennet MD “ Most children who wet the bed have at least one parent or another close relative who had the same problem as a child” (https://howardjbennett.com/medical-articles/bedwetting-questions-answers/)
To back this up, scientists have found some genes that have been shown to lead to delayed night-time bladder control, https://www.ncbi.nlm.nih.gov/pubmed/9152831
So it’s fair to conclude that in most cases, there is a hereditary, genetic link to Enuresis. It often runs in the family.
Treatment Methods
There are quite a few treatment methods available for Enuresis, ranging from medication all the way through to Psychotherapy. Considering the fact that up to 90% of Enuresis in children is the result of them being unusually deep sleepers, and the most successful treatment for this has been positive re-enforcement behavioural modification combined with an alarm system. Some of the treatment methods could be viewed as extreme.
Bedwetting Alarms
Bedwetting alarms are a common, and cheap treatment option. Their purpose is to make a loud noise as soon as they sense a drop of urine and wake up the child. In general there are three types of bedwetting alarm;
Buzzers—Bedwetting alarms that are connected to the body
These alarms are attached to the child’s night-time clothing, usually by a clip. The alarm is then attached to a sensor using a cable. The sensor is placed the child’s underwear so it is ready to react to the first signs of urine, and trigger the attached alarm.
These alarms tend to be inexpensive, but they have their disadvantages; because they are physically attached to the child’s night-time clothing, and underwear using a wire, they are often very uncomfortable, and un-reliable; as the child moves during sleep, they can become detached. They can also cause irritation due to the sensor rubbing against the child’s skin during sleep.
Wireless buzzers
These alarms are similar to the wired buzzers, but instead of the alarm being connected to the sensor with a wire, the sensor communicates with alarm using a radio signal instead. These alarms still tend to be uncomfortable for the child because they still have the sensor attached to their underwear, the sensors also tend to be larger because they have the addition of a radio transmitter built into them.
Bell and pad alarms
These alarms use a detector pad that is placed underneath the child’s bedsheets, instead of a buzzer attached to the child’s night-time clothing. The detector pad usually connects to the alarm with a wire. These types of alarm system tend be more comfortable, and safer than other systems; there isn’t anything attached to the child’s clothing, and there isn’t a wire between the child’s clothing and the device which may get tangled up. The down side to these types of alarm system is that they tend to be the more expensive option.
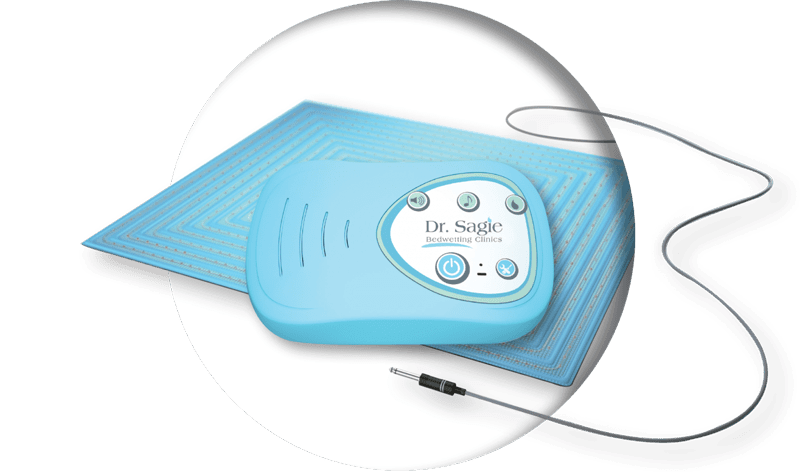
The STOPEE bedwetting alarm is a bell and pad alarm, consisting of a detector pad, and alarm module. This is the most advanced type of alarm currently available.
Medication
Antidiuretics are a class of drug that alter, and control the fluid balance in the body. They are sometimes prescribed treatment for Enuresis, when a doctor has identified that the child does not produce enough of a hormone called ADH (antidiuretic hormone). It must be stresses that the use of medication to treat Enuresis is usually a last resort. This is because Enuresis, in the vast majority of cases can be successfully treated by other means, such as tone of the alarm systems mentioned above. Medication also carries a significant risk of unwanted side effects.
Overview of medications available for bedwetting
DDAVP
Antidiuretic hormone (ADH) is a substance that the body creates naturally to control fluid levels in the body. DDAVP is a synthetic version of this substance, used to inhibit the amount of urine created by the body. In Enuresis cases, it is usually used as a stopgap simply to help children attend sleepovers and camps. It is not intended to be used as a long term solution, it also has side effects such as headaches, runny noses, and nosebleeds. It is available as either a nose spray, or as a pill.
Tofranil
Tofranil is an antidepressant that is known to have a relaxing effect on the bladder. This enables the bladder to hold more urine, making it less likely the child will need to go to the toilet during the night. It has been used as a treatment for Enuresis for around 30 years.
It has some known side effects that tend to manifest when the incorrect dosage is administered:
- Nervousness
- Anxiety
- Constipation
- Personality changes
- A warning: Tofranil can have toxic side effects if taken improperly. Deaths have been attributed to accidental overdoses
Ditropan and Levsin
These two drugs have the effect of reducing unwanted bladder contractions. They are also known to have undesireable side effects that may include:
- Dry mouth
- Drowsiness
- Flushing
- Heat sensitivity
- Constipation
Alternative Treatments
Homeopathy, Reflexology, Acupuncture, Shiatsu, Hypnosis, and fluid restricted diets are all alternative treatment methods that have been tried for Enuresis. However, the fact remains that none have proved to be more successful than the conventional methods, such as alarms and behavioural modification therapy.
Behavioural treatment
The primary purpose of a bedwetting alarm is to stimulate the child to modify their behaviour by training the subconscious continence mechanism. It is not simply intended to wake them up. This is a misconception. Many parents give up on the alarm systems when their child does not respond to it by waking up, they should be aware that even though the child hasn’t awoken, the alarm is fulfilling its purpose because it is acting on their subconscious. In these situations, the parent should persist with using the alarm.
Using an alarm system to modify the child’s behaviour has proven to be more effective than medication in studies; The Journal of Urology, 166, 2427-2431 compared the effectiveness of two popular drugs used to treat Enuresis (Desmopressin and Oxybutynin), versus the use of an alarm in developing children. The study found that after 12 months, 56% of the children using an alarm system were dry, only 18% of the group using desmopressin, and 16% of the group using oxybutynin were dry over the same period.
By combining an alarm system, with the positive behavioural reinforcement techniques employed in the THERApee interactive online software. The THERApee system has achieved success rates of up to 90%. Much higher than simply using an alarm system on its own, or medication.
Understanding the child
It is important that parents make an effort to understand a child’s bedwetting problem, and seek to motivate them to overcome it, rather than simply dismissing the problem, or even worse, making the child feel guilty, or that it is their fault. If it’s not approached and treated properly, it can lead to further social issues for the child as they get older. They will be reluctant to attend sleepovers or camp out with friends, and in some cases, it may lead to them being bullied.
Enuresis is treatable, behavioural modification, using an alarm system has proven to be the most effective method to date. Dr Sagie’s THERApee system is the most complete, and comprehensive treatment plan currently on the market, with over 30,000 successful patients so far and counting.